Part D. Chapter 6: Cross-Cutting Topics of Public Health Importance
What is the relationship between intake of saturated fat and risk of cardiovascular disease?
Conclusion Statements: Strong and consistent evidence from RCTs shows that replacing SFA with unsaturated fats, especially PUFA, significantly reduces total and LDL cholesterol. Replacing SFA with carbohydrates (sources not defined) also reduces total and LDL cholesterol, but significantly increases triglycerides and reduces HDL cholesterol.
Strong and consistent evidence from RCTs and statistical modeling in prospective cohort studies shows that replacing SFA with PUFA reduces the risk of CVD events and coronary mortality. For every 1 percent of energy intake from SFA replaced with PUFA, incidence of CHD is reduced by 2 to 3 percent. However, reducing total fat (replacing total fat with overall carbohydrates) does not lower CVD risk. Consistent evidence from prospective cohort studies shows that higher SFA intake as compared to total carbohydrates is not associated with CVD risk.
DGAC Grade: Strong
Evidence is limited regarding whether replacing SFA with MUFA confers overall CVD (or CVD endpoint) benefits. One reason is that the main sources of MUFA in a typical American diet are animal fat, and because of the co-occurrence of SFA and MUFA in foods makes it difficult to tease out the independent association of MUFA with CVD. However, evidence from RCTs and prospective studies has demonstrated benefits of plant sources of monounsaturated fats, such as olive oil and nuts on CVD risk.
DGAC Grade: Limited
Review of Evidence
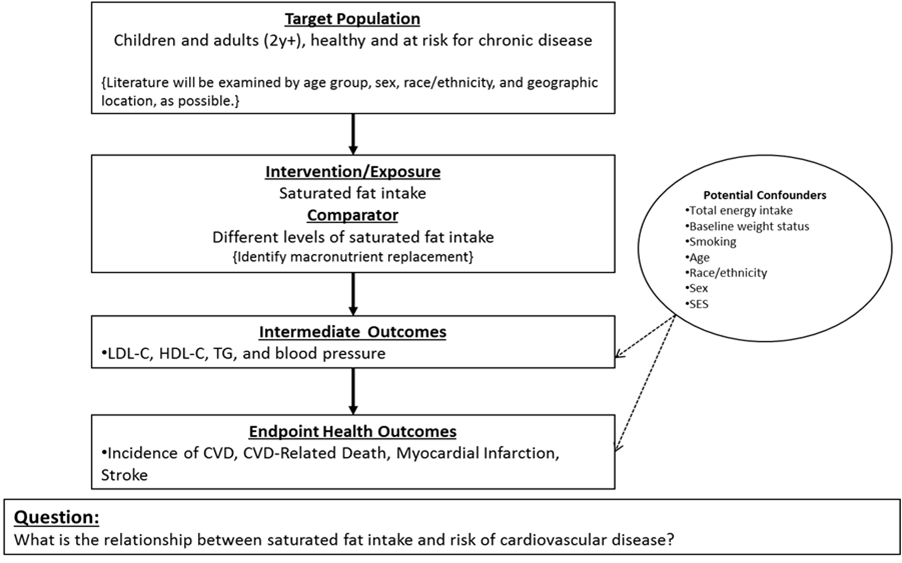
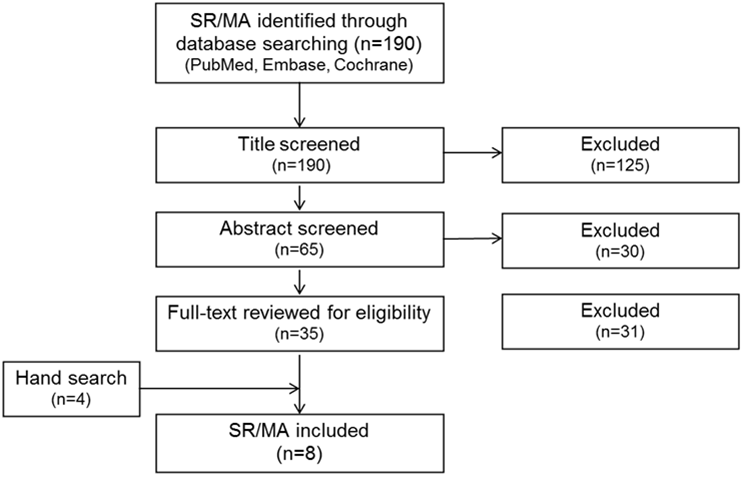
The Committee drew evidence from SRs or MA published between January 2009 and August 2014 in English in a peer-reviewed journal, which included RCTs and/or prospective cohort studies. Participants included healthy volunteers as well as individuals at elevated chronic disease risk. The main exposure was SFA, and the main outcomes included LDL-cholesterol (LDL-C), HDL-cholesterol (HDL-C), triglycerides (TG), blood pressure (BP), and incidence of CVD, CVD-related death, myocardial infarction, or stroke. All reviews were high-quality, with ratings ranging from 8 to 11 on AMSTAR. The Committee drew evidence on blood lipids and blood pressure outcomes from the 2013 AHA/ACC Guideline on Lifestyle Management to Reduce Cardiovascular Risk and the NHLBI Evidence Report on Lifestyle Interventions to Reduce Cardiovascular Disease Risk1, which included primarily RCTs on intermediate CVD risk factors. The Committee drew evidence on CVD endpoints and effect size estimates from seven published MA that included one or more studies not covered in these reports.2 3 4 5 6 7 8 Little evidence on the contribution of SFA to cardiovascular risk factors in the pediatric populations was available, and that which was published has not been systematically reviewed.
Effects of Replacing SFA on LDL-C, HDL-C, and TG
Macronutrients may affect plasma lipids and lipoproteins, which are strong predictors of CVD risk. The NHLBI Lifestyle Report summarized evidence from three feeding trials examining effects on LDL-C of dietary patterns with varying SFA levels: DASH (Dietary Approaches to Stop Hypertension), DASH-Sodium, and DELTA (Dietary Effects on Lipoproteins and Thrombogenic Activity). The results from these trials indicate that reducing total and saturated fat led to a significant reduction in LDL cholesterol in the context of the DASH dietary pattern and the National Cholesterol Education Program (NCEP) Step 1 diet. To estimate the effects of replacing SFA by specific macronutrients such as carbohydrates, MUFA, or PUFA, the NHLBI Lifestyle Report also included two MA from Mensink and Katan (n=1,672), covering the period from 1970 to 1998 (27 controlled trials in the first MA and 60 controlled trials in the second MA) and using the same inclusion/exclusion criteria to estimate changes in plasma lipids when substituting dietary SFA with carbohydrates or other fat types and holding dietary cholesterol constant.9 10 Mensink and Katan found that replacing 1 percent of SFA with an equal amount of carbohydrates, MUFA, or PUFA led to comparable LDL-C reductions: 1.2, 1.3, and 1.8 mg/dL, respectively. Replacing 1 percent of SFA with carbohydrates, MUFA, or PUFA also lowered HDL-C by 0.4, 1.2, and 0.2 mg/dL, respectively. Replacing 1 percent of carbohydrates by an equal amount of MUFA or PUFA raised LDL-C by 0.3 and 0.7 mg/dL, raised HDL-C by 0.3 and 0.2 mg/dL, and lowered TG by 1.7 and 2.3 mg/dL, respectively. The 2003 MA by Mensink and Katan10 indicated that the ratio of total to HDL-C, a stronger predictor of CVD risk than total or LDL cholesterol alone, did not change when SFA was replaced by carbohydrates, but the ratio significantly decreased when SFA was replaced by unsaturated fats, especially PUFA.
In summary, strong and consistent evidence from RCTs shows that replacing SFA with unsaturated fats, especially PUFA, significantly reduces total and LDL cholesterol. Replacing SFA with carbohydrates also reduces total and LDL cholesterol, but significantly increases TG and reduces HDL cholesterol. However, the evidence of beneficial effects on one risk factor does not rule out neutral or opposite effects on unstudied risk factors. To better assess the overall effects of intervention to reduce or modify SFA intake, studies of clinical endpoints are summarized below.
The Relationship between Consumption of Total Fat and SFA and Risk of CVD
A MA by Skeaff et al. in 2009 included 28 U.S. and European cohorts (6,600 CHD deaths among 280,000 participants) and found no clear relationship between total or SFA intake and CHD events or deaths.8 Similarly, Siri-Tarino et al., 2010 found that SFA intake was not associated with risk of CHD, stroke or cardiovascular disease.7 The Siri-Tarino et al., 2010 meta-analysis included data from 347,747 participants (11,006 developed CVD) in 21 unique studies, with 16 studies providing risk estimates for CHD and 8 studies providing data for stroke as an endpoint. In the 2012 MA of trials to reduce or modify intake of SFA, Hooper et al. also found no significant associations of total fat reduction with cardiovascular events or mortality. Consistent with these prior studies, Chowdhury et al.’s 2014 MA of total SFA also did not specify what macronutrient substituted SFA and again found no association of dietary SFA intake, nor of circulating SFA, with coronary disease.2 Chowdhury et al. included data from 32 observational studies (530,525 participants) of fatty acids from dietary intake, 17 observational studies (25,721 participants) of fatty acid biomarkers, and 27 RCTs (103,052 participants) of fatty acid supplementation.
The results described above do not explicitly specify the comparison or replacement nutrient, but typically it consists largely of carbohydrates (sources not defined). These results suggest that replacing SFA with carbohydrates is not associated with CVD risk. Taken together, these results suggest that simply reducing SFA or total fat in the diet by replacing it with any type of carbohydrates is not effective in reducing risk of CVD.
Effects of Replacing SFA with Polyunsaturated Fat or Carbohydrates on CVD Events
Hooper et al.’s 2012 Cochrane MA of trials of SFA reduction/modification found that reducing SFA by reducing and/or modifying dietary fat reduced the risk of cardiovascular events by 14 percent (pooled RR = 0.86; 95% CI = 0.77 to 0.96, with 24 comparisons and 65,508 participants of whom 7 percent had a cardiovascular event, I= 50%).4 Subgroup analyses revealed this protective effect was driven by dietary fat modification rather than reduction and was only apparent in longer trials (2 years or more). Despite the reduction in total cardiovascular events, there was no clear evidence of reductions in any individual outcome (total or non-fatal myocardial infarction, stroke, cancer deaths or diagnoses, diabetes diagnoses), nor was there any evidence that trials of reduced or modified SFA reduced cardiovascular mortality. These results suggest that modifying dietary fat by replacing some saturated (animal) fats with plant oils and unsaturated spreads may reduce risk of heart and vascular disease.
Emphasizing the benefits of replacement of saturated with polyunsaturated fats, Mozaffarian et al., 2010 found in a MA of 8 trials (13,614 participants with 1,042 CHD events) that modifying fat reduced the risk of myocardial infarction or coronary heart disease death (combined) by 19 percent (RR = 0.81; 95% CI = 0.70 to 0.95; p = 0.008), corresponding to 10 percent reduced CHD risk (RR = 0.90; 95% CI = 0.83 to 0.97) for each 5 percent energy of increased PUFA.6 This magnitude of effect is similar to that observed in the Cochrane MA. In secondary analyses restricted to CHD mortality events, the pooled RR was 0.80 (95% CI = 0.65 to 0.98). In subgroup analyses, the RR was greater in magnitude in the four trials in primary prevention populations but non-significant (24 percent reduction in CHD events) compared to a significant reduction of 16 percent in the four trials of secondary prevention populations. Mozaffarian et al. argue that the slightly greater risk reduction in studies of CHD events, compared with predicted effects based on lipid changes alone, is consistent with potential additional benefits of PUFA on other non-lipid pathways of risk, such as insulin resistance. Many of the included trials used vegetable oils containing small amounts of plant-derived n-3 PUFA in addition to omega-6 PUFA.
Consistent with the benefits of replacing SFA with PUFA for prevention of CHD shown in other studies, Farvid et al., 2014 conducted an SR and MA of prospective cohort studies of dietary linoleic acid (LA), which included 13 studies with 310,602 individuals and 12,479 total CHD events (5,882 CHD deaths).3 Farvid et al. found dietary LA intake is inversely associated with CHD risk in a dose-response manner: when comparing the highest to the lowest category of intake, LA was associated with a 15 percent lower risk of CHD events (pooled RR = 0.85; 95% CI = 0.78 to 0.92; I²=35.5%) and a 21% lower risk of CHD deaths (pooled RR = 0.79; 95% CI = 0.71 to 0.89; I²=0.0%). A 5 percent of energy increment in LA intake replacing energy from SFA intake was associated with a 9 percent lower risk of CHD events (RR = 0.91; 95% CI = 0.86 to 0.96) and a 13 percent lower risk of CHD deaths (RR = 0.87; 95% CI = 0.82 to 0.94). In the meta-analysis conducted by Chowdhury et al., there was no significant association between LA intake and CHD risk, but the analysis was based on a limited number of prospective cohort studies.
In Jakobsen et al.’s 2009 pooled analysis of 11 cohorts (344,696 persons with 5,249 coronary events and 2,155 coronary deaths), a 5 percent lower energy intake from SFAs and a concomitant higher energy intake from PUFAs reduced risk of coronary events by 13 percent (hazard ratio [HR] = 0.87; 95% CI = 0.77 to 0.97) and coronary deaths by 16 percent (hazard ratio = 0.74; 95% CI = 0.61 to 0.89).5 By contrast, a 5 percent lower energy intake from SFAs and a concomitant higher energy intake from carbohydrates, there was a modest significant direct association between carbohydrates and coronary events (hazard ratio = 1.07; 95% CI = 1.01 to 1.14) and no association with coronary deaths (hazard ratio = 0.96; 95% CI = 0.82 to 1.13). Notably, the estimated HRs for carbohydrate intake in this study could reflect high glycemic carbohydrate intake rather than total carbohydrate, as fiber was controlled for in the analyses. MUFA intake was not associated with CHD incidence or death.
Taken together, strong and consistent evidence from RCTs and statistical modeling in prospective cohort studies shows that replacing SFA with PUFA reduces the risk of CVD events and coronary mortality. For every 1 percent of energy intake from SFA replaced with PUFA, incidence of CHD is reduced by 2 to 3 percent. The evidence is not as clear for replacement by MUFA or replacement with carbohydrate, and likely depends on the type and source.
Methodological Issues
When individuals in natural settings reduce calories from SFA, they typically replaced them with other macronutrients, and the type and source of the macronutrients substituting SFA determine effects on CVD. For this reason, studies specifying the macronutrient type replacing SFA are more informative than those examining only total SFA intake, and the strongest and most consistent evidence for CVD reduction is with replacement of SFA with PUFA in both RCTs and observational studies.
The differing effects of the type and source of macronutrient substituted may be one reason for the limited evidence regarding whether replacing SFA with MUFA confers CVD benefits and the lack of benefit from carbohydrate substitution. The main sources of MUFA in a typical American diet are animal fats, which could confound potential benefits of SFA-replacement with plant-source MUFA, such as nuts and olive oil, which have demonstrated benefits on CVD risk. To date, evidence testing replacement of SFA by MUFA from different sources is insufficient to reach a firm conclusion. Similarly, most analyses did not distinguish between substitution of saturated fat by different types of carbohydrates (e.g., refined carbohydrate vs. whole grains).
Of the RCTs included in this evidence summary, the intervention methods used varied from long-term dietary counseling with good generalizability but variable compliance, to providing a whole diet for weeks (e.g., controlled feeding studies) with maximal compliance but limited generalizability. Though the content of the recommended or provided diet is known with greater precision in the RCTs than in observational studies, adherence to the diet is likely variable and could result in lack of compliance and high rates of dropout in long-term trials. Additionally, bias may arise from the lack of blinding in non-supplement dietary intervention trials.
In prospective observational studies, misclassification of dietary fatty acid intake could bias associations towards the null. In addition, residual confounding by other dietary and lifestyle factors cannot be ruled out through statistical adjustment. Despite these methodological issues, there is high consistency of the evidence from prospective cohort studies and RCTs in supporting the benefits of replacing saturated fat with unsaturated fats especially PUFA in reducing CVD risk.
Table 1. Summary of existing reports, systematic reviews, and meta-analyses examining the relationship between the intake of saturated fat and risk of cardiovascular disease
|
Author, Year Publication Type AMSTAR Rating* |
Independent Variable Outcomes Considered |
Date Range Searched Criteria Used |
Included Studies** (Number and Design) |
Recommendations, Evidence/Conclusion Statements, and/or Main Results from Existing Report/ SR/ MA |
|---|---|---|---|---|
|
NHLBI, 2013; Eckel, 2014 Systematic Review AMSTAR: 9/11 |
Examined “dietary patterns”; focused on studies that assessed macronutrients (types and amount), including SFAs (discussed replacement) Plasma LDL-C, HDL-C, and TG |
1998-2009 for trials; 1990-2009 for SR/MA Trials with minimum of 1 mo of exposure; any geographic location and clinical or research setting; adults (≥18 years of age) with or without established CVD; with or without CVD risk factors; with or without tobacco use; and who were of normal weight, overweight, or obese; studies were excluded if they focused on the use of dietary supplements or non-oral routes of nutrient delivery or the primary outcome of the nutritional intervention was weight change or when the weight change was greater than 3% |
5 trials (6 papers); four systematic reviews/meta-analyses (2 were used to inform evidence statements; one had 27 RCTs; one had 60 trials) |
Recommendations (AHA/ACC): Advise adults who would benefit from LDL–C lowering to:
Evidence Statements (NHLBI): ES11. When food was supplied to adults in a dietary pattern that achieved a macronutrient composition of 5–6 % saturated fat, 26–27 % total fat, 15–18 % protein, and 55–59 % carbohydrates, compared with a control diet (14–15% saturated fat, 34–38% total fat, 13–15% protein, and 48–51% carbohydrate), LDL-C was lowered 11–13mg/dL in two studies and 11 % in one study. Strength of evidence: High ES12. In controlled feeding trials among adults, for every 1% of energy from SFA that is replaced by 1% of energy from carbohydrate, MUFA, or PUFA:
For every 1% of energy from SFA that is replaced by 1% of energy from:
Strength of evidence: Moderate ES13. In controlled feeding trials among adults, for every 1% of energy from carbohydrates that is replaced by 1% of energy from:
Strength of evidence: Moderate |
|
Hooper, 2012 Systematic Review AMSTAR: 11/11 |
Examined reduction and/or modification of dietary fats, including SFAs (discussed replacement) Cardiovascular mortality and events (MI, stroke, angina, heart failure, peripheral vascular disease, angioplasty, and coronary artery bypass grafting) |
Up to June 2010 RCTs of at least 6 mo duration; intention to reduce or modify fat intake (excluding exclusively omega-3 fat interventions); not multi-factorial; adult humans with or without CVD, but excluding those who were acutely ill, pregnant, or lactating |
48 RCTs (some trials included multiple papers) |
Conclusions: Findings are suggestive of a small but potentially important reduction in cardiovascular risk on modification of dietary fat, but not reduction of total fat, in longer trials. Lifestyle advice to all those at risk of CVD and to lower risk population groups, should continue to include permanent reduction of dietary saturated fat and partial replacement by unsaturates. The ideal type of unsaturated fat is unclear. Main results: This updated review suggested that reducing saturated fat by reducing and/or modifying dietary fat reduced the risk of cardiovascular events by 14%. Subgrouping suggested that this reduction in cardiovascular events was seen in studies of fat modification (not reduction-which related directly to the degree of effect on serum total and LDL cholesterol and triglycerides), of at least two years duration and in studies of men (not of women). There were no clear effects of dietary fat changes on cardiovascular mortality. |
|
Mozaffarian, 2010 Meta-Analysis AMSTAR: 11/11 |
Examined PUFA consumption, as a replacement for SFA Incidence of CHD (MI and/or cardiac death) |
Up to June 2009 RCTs of at least 1 yr duration; without concomitant interventions; appropriate control group |
8 RCTs |
Conclusions: These findings provide evidence that consuming PUFA in place of SFA reduces CHD events in RCTs. This suggests that rather than trying to lower PUFA consumption, a shift toward greater population PUFA consumption in place of SFA would significantly reduce rates of CHD. Main results: Average weighted PUFA consumption was 14.9% energy in intervention groups versus 5.0% energy in controls. The overall pooled risk reduction was 19%, corresponding to 10% reduced CHD risk for each 5% energy of increased PUFA, without evidence for statistical heterogeneity. |
|
Siri-Tarino, 2010 Meta-Analysis AMSTAR: 9/11 |
Examined SFA (insufficient power to assess effects of replacing SFAs with PUFAs or CHO) Nonfatal or fatal CVD (but not CVD risk factors) |
Up to September 2009 PCSs that specifically evaluated SFAs and CVD among generally healthy adults at baseline |
21 PCSs |
Conclusions: A meta-analysis of prospective epidemiologic studies showed that there is no significant evidence for concluding that dietary saturated fat is associated with an increased risk of CHD or CVD. More data are needed to elucidate whether CVD risks are likely to be influenced by the specific nutrients used to replace saturated fat. Main results: Intake of saturated fat was not associated with an increased risk of CHD, stroke, or CVD. The pooled relative risk estimates that compared extreme quantiles of saturated fat intake were 1.07 for CHD, 0.81 for stroke, and 1.00 for CVD. Consideration of age, sex, and study quality did not change the results. |
|
Chowdhury, 2014 Systematic Review and Meta-Analysis AMSTAR: 11/11 |
Examined SFA, MUFAs, and PUFAs, but did not assess replacement Coronary events |
Up to July 2013 PCSs with at least 1 yr with participants from the general population or with stable CVD at study entry |
20 PCSs (25 papers) with SFA |
Conclusions: Current evidence does not clearly support cardiovascular guidelines that encourage high consumption of polyunsaturated fatty acids and low consumption of total saturated fats. Main results: Relative risks for coronary disease were 1.02 for saturated, 0.99 for monounsaturated, 0.93 for long-chain n-3 polyunsaturated, 1.01 for n-6 polyunsaturated, and 1.16 for trans fatty acids when the top and bottom thirds of baseline dietary fatty acid intake were compared. |
|
Farvid, 2014 Meta-Analysis AMSTAR: 9/11 |
Examined dietary linoleic acid, including replacing SFAs with linoleic acid (LA) CHD outcomes (MI, ischemic heart disease, coronary artery bypass graft, sudden cardiac arrest, acute coronary syndrome and CHD deaths) |
Up to June 2013 PCSs in adults that provided multivariate-adjusted risk estimates or hazard ratios for dietary LA and CHD endpoints; excluded retrospective, cross-sectional, ecological studies; excluded meeting abstracts and duplicated publications; excluded studies in patients with known CHD at baseline; for papers from the same cohort, used the most recent analyses with the highest number of outcomes |
8 PCSs examined substitution of LA for SFA |
Conclusions: These data provide support for current recommendations to replace saturated fat with polyunsaturated fat for primary prevention of CHD in the general population. Main results: A 5% of energy increment in linoleic acid intake replacing energy from saturated fat intake was associated with a 9% lower risk of CHD events and a 13% lower risk of CHD deaths. |
|
Jakobsen, 2009 Meta-Analysis (Pooled analysis) AMSTAR: 8/11 |
Examined replacement of SFAs with MUFAs, PUFAs, or CHO Fatal CHD (including sudden death) and nonfatal MI |
Not specified Studies that included a published follow-up study with at least 150 incident coronary evident; availability of usual dietary intake; validation of diet assessment method; excluded persons who were <35 yrs, had a history of CVD, diabetes, or cancer, or had extreme energy intake |
11 cohorts (9 PCSs and 2 randomized primary prevention studies) |
Conclusions: The findings suggest that replacing SFAs with PUFAs rather than MUFAs or carbohydrates prevents CHD over a wide range of intakes. Main results: For a 5% lower energy intake from SFAs and a concomitant higher energy intake from PUFAs, there was a significant inverse association between PUFAs and risk of coronary events (hazard ratio: 0.87; 95% CI: 0.77 to 0.97); the hazard ratio for coronary deaths was 0.74 (95% CI: 0.61 to 0.89). For a 5% lower energy intake from SFAs and a concomitant higher energy intake from carbohydrates, there was a modest significant direct association between carbohydrates and coronary events (hazard ratio: 1.07; 95% CI: 1.01 to 1.14); the hazard ratio for coronary deaths was 0.96 (95% CI: 0.82 to 1.13). MUFA intake was not associated with CHD. No effect modification by sex or age was found. |
|
Skeaff, 2009 Meta-Analysis AMSTAR: 8/11 |
Examined dietary fat, including total fat, SFAs, TFAs, MUFAs, and PUFAs, but did not assess replacement CHD death, CHD events, and non-fatal CHD |
Not specified Cohort studies and controlled trials; English language |
11 cohorts (12 papers) in SFA analysis |
Main results: Intake of SFA was not significantly associated with CHD mortality, with a RR of 1.14 (p =0.431) for those in the highest compared with the lowest category of SFA intake. Similarly, SFA intake was not significantly associated with CHD events (RR 0.93, p = 0.269 for high vs. low categories). Moreover, there was no significant association with CHD death (RR 1.11, p = 0.593) per 5% total energy increment in SFA intake. For the cohort studies included in the meta-analysis, mean or median SFA intake varied from 7 to 11% total energy in the lowest category to 14 to 18% total energy in the highest category. Overall the mean or median SFA intake in all cohort studies varied from 9 to 20% total energy. |
* A measurement tool for the ‘assessment of multiple systematic reviews’ (AMSTAR)
** Reference overlap: In total, 166 articles were considered in these reviews, of which 24 were included in two or more reviews.
References Included in Review
- National Heart, Lung, and Blood Institute. Lifestyle interventions to reduce cardiovascular risk: Systematic evidence review from the Lifestyle Work Group, 2013. Bethesda, MD: U.S. Department of Health and Human Services, National Institutes of Health, 2013. http://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/lifestyle/index.htm
Associated Lifestyle Guideline:
Eckel RH, Jakicic JM, Ard JD, de Jesus JM, Houston Miller N, Hubbard VS, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014 Jun 24;129(25 Suppl 2):S76-99. doi: 10.1161/01.cir.0000437740.48606.d1. Epub 2013 Nov 12. PubMed PMID: 24222015. http://www.ncbi.nlm.nih.gov/pubmed/24222015 - Chowdhury R, Warnakula S, Kunutsor S, Crowe F, Ward HA, Johnson L, et al. Association of dietary, circulating, and supplement fatty acids with coronary risk: a systematic review and meta-analysis. Ann Intern Med. 2014;160(6):398-406. PMID: 24723079. http://www.ncbi.nlm.nih.gov/pubmed/24723079
- Farvid MS, Ding M, Pan A, Sun Q, Chiuve SE, Steffen LM, Willett WC, Hu FB. Dietary linoleic acid and risk of coronary heart disease: A systematic review and meta-analysis of prospective cohort studies. Circulation. 2014 Aug 26. pii: CIRCULATIONAHA.114.010236. [Epub ahead of print] PubMed PMID: 25161045. http://www.ncbi.nlm.nih.gov/pubmed/25161045
- Hooper L, Summerbell CD, Thompson R, Sills D, Roberts FG, Moore HJ, et al. Reduced or modified dietary fat for preventing cardiovascular disease. Cochrane Database Syst Rev. 2012;5:CD002137. PMID: 22592684. http://www.ncbi.nlm.nih.gov/pubmed/22592684
- Jakobsen MU, O'Reilly EJ, Heitmann BL, Pereira MA, Bälter K, Fraser GE, Goldbourt U, Hallmans G, Knekt P, Liu S, Pietinen P, Spiegelman D, Stevens J, Virtamo J, Willett WC, Ascherio A. Major types of dietary fat and risk of coronary heart disease: a pooled analysis of 11 cohort studies. Am J Clin Nutr. 2009 May;89(5):1425-32. doi: 10.3945/ajcn.2008.27124. Epub 2009 Feb 11. PubMed PMID: 19211817; PubMed Central PMCID: PMC2676998. http://www.ncbi.nlm.nih.gov/pubmed/19211817
- Mozaffarian D, Micha R, Wallace S. Effects on coronary heart disease of increasing polyunsaturated fat in place of saturated fat: a systematic review and meta-analysis of randomized controlled trials. PLoS Med. 2010;7(3):e1000252. PMID: 20351774. http://www.ncbi.nlm.nih.gov/pubmed/20351774
- Siri-Tarino PW, Sun Q, Hu FB, Krauss RM. Meta-analysis of prospective cohort studies evaluating the association of saturated fat with cardiovascular disease. Am J Clin Nutr. 2010;91(3):535-46. PMID: 20071648. http://www.ncbi.nlm.nih.gov/pubmed/20071648
- Skeaff CM, Miller J. Dietary fat and coronary heart disease: summary of evidence from prospective cohort and randomised controlled trials. Ann Nutr Metab. 2009;55(1-3):173-201. doi: 10.1159/000229002. Epub 2009 Sep 15. PubMed PMID: 19752542. http://www.ncbi.nlm.nih.gov/pubmed/19752542
Additional References
- Mensink RP, Katan MB. Effect of dietary fatty acids on serum lipids and lipoproteins. A meta-analysis of 27 trials. Arterioscler Thromb. 1992;12(8):911-9. PMID: 1386252. http://www.ncbi.nlm.nih.gov/pubmed/1386252.
- Mensink RP, Zock PL, Kester AD, Katan MB. Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials. Am J Clin Nutr. 2003;77(5):1146-55. PMID: 12716665. http://www.ncbi.nlm.nih.gov/pubmed/12716665.
Supplementary Information
Analytical Framework
Methodology
This question was answered using the National Heart, Lung, and Blood Institute Systematic Evidence Review from the Lifestyle Work Group, 2013 and related AHA/ACC Guideline on Lifestyle Management to Reduce Cardiovascular Risk,1 which focused on randomized controlled trials (RCTs), as well as existing SRs and MA addressing this question published in peer-reviewed literature between January 2009 and August 2014. Particular emphasis was placed on reviews that examined the macronutrient replacement for saturated fat.
Search Strategy for Existing Systematic Reviews/Meta-Analyses
PubMed:
"Mortality"[Mesh] OR mortality[tiab] OR "blood pressure"[tiab] OR "blood pressure"[mesh] OR "cardiovascular diseases"[mh:noexp] OR cardiovascular disease*[tiab] OR cardiovascular event*[tiab] OR hypertension[tiab] OR "Myocardial Infarction"[Mesh] OR "Myocardial Infarction"[tiab] OR "Heart Failure"[Mesh] OR "Heart Arrest"[Mesh] OR "Myocardial Ischemia"[Mesh] OR "heart failure"[tiab] OR "heart arrest"[tiab] OR "Myocardial Ischemia"[tiab] OR hypertension[mh] OR stroke[tiab] OR "stroke"[Mesh] OR mortality[sh] OR (coronary[tiab] AND disease*[tiab])
OR
"cholesterol/blood"[mh] OR "Cholesterol, Dietary"[Mesh] OR "Cholesterol"[Mesh] OR "Cholesterol, HDL"[Mesh] OR "Cholesterol, LDL"[Mesh] OR "Cholesterol, VLDL"[Mesh] OR cholesterol[tiab] OR "Cholesterol, Dietary"[Mesh] OR triglyceride* OR "Lipids/blood"[Mesh] OR hypercholesterolemia[mh] OR hypercholesterol*[tiab] OR hypercholesterolemia[tiab]
AND
(saturated AND ("Fatty Acids"[Mesh] OR "Dietary Fats"[Mesh] OR fat[tiab] OR fats[tiab] OR fatty[tiab])) OR saturated-fat[tiab]
OR
Meat[tiab] OR dairy[tiab] OR milk[tiab] OR butter[tiab] OR yogurt[tiab] OR cheese*[tiab] OR"Dairy Products"[Mesh] OR "Meat"[Mesh] OR meat[tiab] OR margarine*[tiab] OR yoghurt*[tiab] OR egg OR eggs
Embase:
'cardiovascular disease'/de OR ‘cardiovascular disease’:ti,ab OR 'hypertension'/exp OR hypertension:ti,ab OR 'blood pressure'/exp OR 'blood pressure':ti,ab OR 'mortality'/exp OR mortality:ti,ab OR 'triacylglycerol'/exp OR triglyceride*:ab,ti OR (cholesterol NEAR/2 (hdl OR ldl)) OR 'low density lipoprotein'/exp OR 'high density lipoprotein cholesterol'/exp OR 'cholesterol intake'/exp OR cholesterol:ti,ab OR 'stroke'/exp OR 'heart failure'/exp OR 'heart failure':ti,ab OR 'heart infarction'/exp OR 'heart infarction':ti,ab OR 'heart disease'/exp OR 'heart disease':ti,ab OR lipid/exp OR lipid*:ti,ab OR 'cholesterol'/exp OR 'cholesterol':ti,ab OR 'meat'/exp OR hyperlipidemia:ti,ab OR hypercholesterolem*:ti,ab OR hypertriglyeridem*:ti,ab
AND
('saturated fatty acid'/exp OR (saturated NEAR/3 (fat OR fatty OR fats)))
OR
'meat':ti,ab OR 'dairy product'/exp OR milk:ti,ab OR cheese:ti,ab OR butter:ti,ab OR ‘ice cream’:ti,ab OR yogurt:ti,ab OR yoghurt:ti,ab OR margarine:ti,ab
AND 'systematic review'/exp OR 'meta analysis'/exp
Cochrane:
mortality OR "blood pressure" OR (cardiovascular NEXT (event OR disease*)) OR coronary NEXT heart NEXT disease* OR ((cholesterol OR lipid*) NEAR/2 blood) OR (Cholesterol NEAR/2 HDL) OR cholesterol OR (Cholesterol NEAR/2 Dietary) OR triglyceride* OR "Myocardial Infarction" OR "Heart Arrest" OR "Myocardial Ischemia" OR "heart failure" OR hypertension OR “Myocardial Infarction" OR “heart arrest” OR “Myocardial Ischemia" OR stroke OR hypercholesterol* OR hypercholesterolemia*
AND
(saturated NEAR/2 (Fatty OR fats OR fat)) OR saturated-fat OR
Meat OR dairy OR milk OR butter OR yogurt OR cheese OR "Meat" OR margarine*OR yoghurt* OR egg*
Inclusion Criteria
Date Range:
- Published between January 2009 and August 2014 (in English in a peer-reviewed journal)
Study Design:
- Systematic review and/or meta-analysis that included randomized controlled trials and/or prospective cohort studies
Study Subjects:
- Reviews that included studies from high or very high human development (2012 Human Development Index)
- Healthy or at elevated chronic disease risk
Intervention/Exposure:
- Saturated fat
Outcome:
- LDL-cholesterol, HDL-cholesterol, triglycerides, blood pressure, incidence of CVD, CVD-related death, myocardial infarction, or stroke
Quality:
- Reviews rated 8-11 on AMSTAR (A measurement tool for the ‘assessment of multiple systematic reviews’)
Search Results
Excluded Articles with Reason for Exclusion
- Abete I, Romaguera D, Vieira AR, Lopez de Munain A, Norat T. Association between total, processed, red and white meat consumption and all-cause, CVD and IHD mortality: a meta-analysis of cohort studies. Br J Nutr. 2014:1-14. PMID: 24932617. http://www.ncbi.nlm.nih.gov/pubmed/24932617. EXCLUDE: Examined food source, not saturated fat specifically
- Astrup A, Dyerberg J, Elwood P, Hermansen K, Hu FB, Jakobsen MU, et al. The role of reducing intakes of saturated fat in the prevention of cardiovascular disease: where does the evidence stand in 2010? Am J Clin Nutr. 2011;93(4):684-8. PMID: 21270379. http://www.ncbi.nlm.nih.gov/pubmed/21270379. EXCLUDE: Article is a Perspective and provides symposium proceedings
- Astrup A. Yogurt and dairy product consumption to prevent cardiometabolic diseases: epidemiologic and experimental studies. Am J Clin Nutr. 2014 May;99(5 Suppl):1235S-42S. doi: 10.3945/ajcn.113.073015. Epub 2014 Apr 2. Review. PubMed PMID: 24695891. http://www.ncbi.nlm.nih.gov/pubmed/24695891. EXCLUDE: Narrative review
- Benatar JR, Sidhu K, Stewart RA. Effects of high and low fat dairy food on cardio-metabolic risk factors: a meta-analysis of randomized studies. PLoS One. 2013;8(10):e76480. PMID: 24146877. http://www.ncbi.nlm.nih.gov/pubmed/24146877. EXCLUDE: Examined food source, not saturated fat specifically
- Chen GC, Lv DB, Pang Z, Liu QF. Red and processed meat consumption and risk of stroke: a meta-analysis of prospective cohort studies. Eur J Clin Nutr. 2013;67(1):91-5. PMID: 23169473. http://www.ncbi.nlm.nih.gov/pubmed/23169473. EXCLUDE: Examined food source, not saturated fat specifically
- De Goede J, Geleijnse JM, Ding EL, Soedamah-Muthu SS. Cheese consumption and blood lipids; a systematic review and meta-analysis of randomized controlled trials. Circulation. 2014;129((De Goede J.; Geleijnse J.M.; Soedamah-Muthu S.S.) Wageningen Univ, Wageningen, Netherlands). EXCLUDE: Abstract only
- Fattore E, Bosetti C, Brighenti F, Agostoni C, Fattore G. Palm oil and blood lipid-related markers of cardiovascular disease: a systematic review and meta-analysis of dietary intervention trials. Am J Clin Nutr. 2014;99(6):1331-50. PMID: 24717342. http://www.ncbi.nlm.nih.gov/pubmed/24717342. EXCLUDE: Examined food source, not saturated fat specifically
- Gibson RA, Makrides M, Smithers LG, Voevodin M, Sinclair AJ. The effect of dairy foods on CHD: a systematic review of prospective cohort studies. Br J Nutr. 2009;102(9):1267-75. PMID: 19682399. http://www.ncbi.nlm.nih.gov/pubmed/19682399. EXCLUDE: Examined food source, not saturated fat specifically
- Hooper L, Summerbell CD, Thompson R, Sills D, Roberts FG, Moore H, et al. Reduced or modified dietary fat for preventing cardiovascular disease. Cochrane Database Syst Rev. 2011(7):CD002137. PMID: 21735388. http://www.ncbi.nlm.nih.gov/pubmed/21735388. EXCLUDE: Included updated review (Hooper et al., 2012)
- Hu D, Huang J, Wang Y, Zhang D, Qu Y. Dairy foods and risk of stroke: a meta-analysis of prospective cohort studies. Nutr Metab Cardiovasc Dis. 2014;24(5):460-9. PMID: 24472634. http://www.ncbi.nlm.nih.gov/pubmed/24472634. EXCLUDE: Examined food source, not saturated fat specifically
- Hunter JE, Zhang J, Kris-Etherton PM. Cardiovascular disease risk of dietary stearic acid compared with trans, other saturated, and unsaturated fatty acids: a systematic review. Am J Clin Nutr. 2010;91(1):46-63. PMID: 19939984. http://www.ncbi.nlm.nih.gov/pubmed/19939984. EXCLUDE: Article focuses on stearic acid specifically
- Kaluza J, Wolk A, Larsson SC. Red meat consumption and risk of stroke: a meta-analysis of prospective studies. Stroke. 2012;43(10):2556-60. PMID: 22851546. http://www.ncbi.nlm.nih.gov/pubmed/22851546. EXCLUDE: Examined food source, not saturated fat specifically
- Kratz M, Baars T, Guyenet S. The relationship between high-fat dairy consumption and obesity, cardiovascular, and metabolic disease. Eur J Nutr. 2013;52(1):1-24. PMID: 22810464. http://www.ncbi.nlm.nih.gov/pubmed/22810464. EXCLUDE: Narrative review
- Larsson SC, Orsini N. Red meat and processed meat consumption and all-cause mortality: a meta-analysis. Am J Epidemiol. 2014;179(3):282-9. PMID: 24148709. http://www.ncbi.nlm.nih.gov/pubmed/24148709. EXCLUDE: Only considered all-cause mortality
- Li Y, Zhou C, Zhou X, Li L. Egg consumption and risk of cardiovascular diseases and diabetes: a meta-analysis. Atherosclerosis. 2013;229(2):524-30. PMID: 23643053. http://www.ncbi.nlm.nih.gov/pubmed/23643053. EXCLUDE: Examined food source, not saturated fat specifically
- Maki KC, Van Elswyk ME, Alexander DD, Rains TM, Sohn EL, McNeill S. A meta-analysis of randomized controlled trials that compare the lipid effects of beef versus poultry and/or fish consumption. J Clin Lipidol. 2012;6(4):352-61. PMID: 22836072. http://www.ncbi.nlm.nih.gov/pubmed/22836072. EXCLUDE: Examined food source, not saturated fat specifically
- Mente A, de Koning L, Shannon HS, Anand SS. A systematic review of the evidence supporting a causal link between dietary factors and coronary heart disease. Arch Intern Med. 2009;169(7):659-69. PMID: 19364995. http://www.ncbi.nlm.nih.gov/pubmed/19364995. EXCLUDE: Unable to identify which studies were considered for each outcome
- Micha R, Wallace SK, Mozaffarian D. Red and processed meat consumption and risk of incident coronary heart disease, stroke, and diabetes mellitus: a systematic review and meta-analysis. Circulation. 2010;121(21):2271-83. PMID: 20479151. http://www.ncbi.nlm.nih.gov/pubmed/20479151. EXCLUDE: Examined food source, not saturated fat specifically
- Mozaffarian D. The great fat debate: taking the focus off of saturated fat. J Am Diet Assoc. 2011;111(5):665-6. PMID: 21515109. http://www.ncbi.nlm.nih.gov/pubmed/21515109. EXCLUDE: Commentary
- O’Sullivan TA, Hafekost K, Mitrou F, Lawrence D. Food sources of saturated fat and the association with mortality: a meta-analysis. Am J Public Health. 2013;103(9):e31-42. PMID: 23865702. http://www.ncbi.nlm.nih.gov/pubmed/23865702. EXCLUDE: Examined food source, not saturated fat specifically
- Ralston RA, Lee JH, Truby H, Palermo CE, Walker KZ. A systematic review and meta-analysis of elevated blood pressure and consumption of dairy foods. J Hum Hypertens. 2012;26(1):3-13. PMID: 21307883. http://www.ncbi.nlm.nih.gov/pubmed/21307883. EXCLUDE: Examined food source, not saturated fat specifically
- Ramsden CE, Zamora D, Leelarthaepin B, Majchrzak-Hong SF, Faurot KR, Suchindran CM, et al. Use of dietary linoleic acid for secondary prevention of coronary heart disease and death: evaluation of recovered data from the Sydney Diet Heart Study and updated meta-analysis. BMJ. 2013;346:e8707. PMID: 23386268. http://www.ncbi.nlm.nih.gov/pubmed/23386268. EXCLUDE: Articles focuses on secondary prevention of coronary heart disease
- Ravnskov U, DiNicolantonio JJ, Harcombe Z, Kummerow FA, Okuyama H, Worm N. The questionable benefits of exchanging saturated fat with polyunsaturated fat. Mayo Clin Proc. 2014;89(4):451-3. PMID: 24581756. http://www.ncbi.nlm.nih.gov/pubmed/24581756. EXCLUDE: Commentary
- Rong Y, Chen L, Zhu T, Song Y, Yu M, Shan Z, et al. Egg consumption and risk of coronary heart disease and stroke: dose-response meta-analysis of prospective cohort studies. BMJ. 2013;346:e8539. PMID: 23295181. http://www.ncbi.nlm.nih.gov/pubmed/23295181. EXCLUDE: Examined food source, not saturated fat specifically
- Salter AM. Dietary fatty acids and cardiovascular disease. Animal. 2013;7 Suppl 1:163-71. PMID: 23031737. http://www.ncbi.nlm.nih.gov/pubmed/23031737. EXCLUDE: Narrative review
- Schwingshackl L, Hoffmann G. Comparison of effects of long-term low-fat vs high-fat diets on blood lipid levels in overweight or obese patients: a systematic review and meta-analysis. J Acad Nutr Diet. 2013;113(12):1640-61. PMID: 24139973. http://www.ncbi.nlm.nih.gov/pubmed/24139973. EXCLUDE: Article focuses on total fat content of the diet; compares low-fat to high-fat diets
- Schwingshackl L, Hoffmann G. Dietary fatty acids in the secondary prevention of coronary heart disease: a systematic review, meta-analysis and meta-regression. BMJ Open. 2014;4(4):e004487. PMID: 24747790. http://www.ncbi.nlm.nih.gov/pubmed/24747790. EXCLUDE: Article focuses on secondary prevention of coronary heart disease
- Shin JY, Xun P, Nakamura Y, He K. Egg consumption in relation to risk of cardiovascular disease and diabetes: a systematic review and meta-analysis. Am J Clin Nutr. 2013;98(1):146-59. PMID: 23676423. http://www.ncbi.nlm.nih.gov/pubmed/23676423. EXCLUDE: Examined food source, not saturated fat specifically
- Soedamah-Muthu SS, Ding EL, Al-Delaimy WK, Hu FB, Engberink MF, Willett WC, et al. Milk and dairy consumption and incidence of cardiovascular diseases and all-cause mortality: dose-response meta-analysis of prospective cohort studies. Am J Clin Nutr. 2011;93(1):158-71. PMID: 21068345. http://www.ncbi.nlm.nih.gov/pubmed/21068345. EXCLUDE: Examined food source, not saturated fat specifically
- Soedamah-Muthu SS, Verberne LD, Ding EL, Engberink MF, Geleijnse JM. Dairy consumption and incidence of hypertension: a dose-response meta-analysis of prospective cohort studies. Hypertension. 2012;60(5):1131-7. PMID: 22987924. http://www.ncbi.nlm.nih.gov/pubmed/22987924. EXCLUDE: Examined food source, not saturated fat specifically
- Stettler N, Murphy MM, Barraj LM, Smith KM, Ahima RS. Systematic review of clinical studies related to pork intake and metabolic syndrome or its components. Diabetes Metab Syndr Obes. 2013;6:347-57. PMID: 24106428. http://www.ncbi.nlm.nih.gov/pubmed/24106428. EXCLUDE: Examined food source, not saturated fat specifically