Part D. Chapter 6: Cross-Cutting Topics of Public Health Importance
What is the relationship between the intake of low-calorie sweeteners (LCS) and measures of body weight/obesity?
Conclusion Statements: Moderate and generally consistent evidence from short-term RCTs conducted in adults and children supports that replacing sugar-containing sweeteners with LCSs reduces calorie intake, body weight, and adiposity.
DGAC Grade: Moderate
Long-term observational studies conducted in children and adults provide inconsistent evidence of an association between LCS and body weight as compared to sugar-containing sweeteners.
DGAC Grade: Limited
Review of Evidence
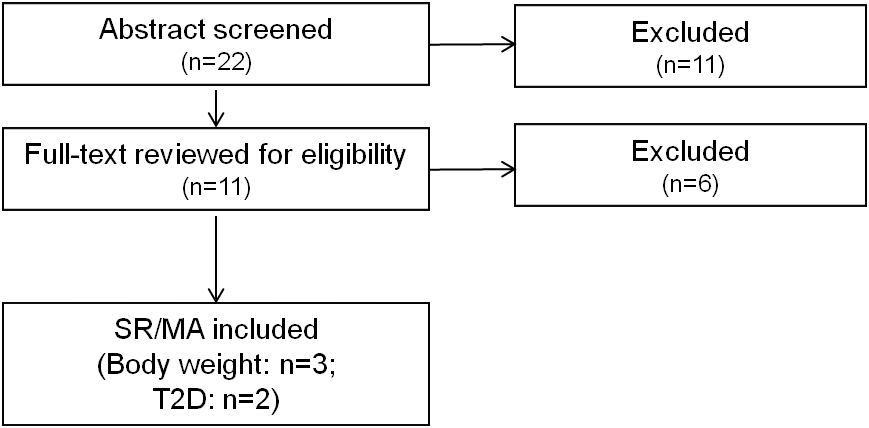
The evidence to support these conclusions comes from three SRs/MA published between January 2010 and August 2014.1 2 3 In total, 39 articles were considered in these reviews, of which six were included in two or more reviews. Experimentally, the protocols described in the 39 articles included RCTs and prospective cohort studies. Although results from both experimental designs were carefully assessed, the DCAC deemed evidence from RCTs to be scientifically stronger and used it as the foundation for conclusions pertaining to body weight.
Among prospective cohort studies, LCS intake was not associated with body weight or fat mass, but was significantly associated with slightly higher BMI (0.03; 95% CI = 0.01 to 0.06).2 These findings should be viewed with caution, however, because of the high risk of reverse causality and the possibility that people with higher body weights would consume more LCS-containing foods and beverages as a weight-control strategy.
Evidence from short-term RCTs consistently indicated that LCSs (vs. sugar-containing foods and beverages) modestly reduces body weight in adults. When evidence from adults and children were combined, LCSs modestly reduced BMI, fat mass, and waist circumference. The primary research articles used by Miller and Perez for the MA contained findings from both adults (n=5 cohorts) and children (n=4 cohorts).2 The results of interventions lasting 3 to 78 weeks indicated that LCSs reduced body weight in adults (-0.72 kg; 95% CI = -1.15 to -0.30) and children (-1.06 kg; 95% CI = -1.17 to -0.56). Age-specific results were not provided for BMI, fat mass, or waist circumference, but data from both age groups were pooled to show the impact of LCSs vs. sugar-containing foods/beverages on these outcomes.
In contrast, Brown et al. summarized that very limited evidence from three short-term (12 to 25 week) RCTs, which suggested that consumption of LCS does not influence body weight or BMI in predominantly pre-teenage and teenage youth (ages 10 to 21 years), compared to sugar-sweetened beverage or placebo.1 The authors cautioned that insufficient data exist to assess causality of LCS on body weight. The evidence reported in this 2010 publication was obtained from very heterogeneous experimental designs and interventions. One study tested the effects of encapsulated aspartame vs. placebo during weight loss; another allowed subjects to exchange sugar-sweetened beverages with either LCS beverages or water (precluding assessment of LCS beverages specifically); and a third was described as a “pilot study.”
Collectively, evidence is mixed on the impact of LCSs vs. sugar-containing foods/beverages on body weight in children. However, the DGAC deemed evidence presented by Miller and Perez to be stronger than from Brown et al. because it culminated from a larger, more recent research base and include both systematic review and meta-analysis assessment and evaluation techniques.
Table 1. Summary of existing reports, systematic reviews, and meta-analyses examining the relationship between the intake of low-calorie sweeteners (LCS) and body weight or risk of obesity
|
Author, Year Publication Type AMSTAR Rating* |
Low-calorie Sweeteners (LCS) Considered Outcomes Considered |
Date Range Searched Criteria Used |
Included Studies** (Number and Design) |
Recommendations, Evidence/Conclusion Statements, and/or Main Results from Existing Report/ SR/ MA |
|---|---|---|---|---|
|
Brown, 2010 Systematic Review AMSTAR: 8/11 |
“Artificial sweeteners” identified by the following terms: artificial sweeteners, sweetening agent, sweetener, sugar substitute, nonnutritive sweetener, intense sweetener, sucralose, aspartame, saccharin, sugar free metabolic health effects, such as food intake, weight change, diabetes, and metabolic syndrome components |
No date restriction (published in 2010) Studies were required to: be published in peer reviewed journals in the English language, include pediatric subjects age 0 to 18; specifically address artificial sweetener consumption in association with metabolic health effects, such as food intake, weight change, diabetes, and metabolic syndrome components; and provide original data. Articles published solely in abstract form were omitted |
18 studies (included 3 RCTs, 6 prospective cohort studies, 3 cross-sectional studies, and 6 food intake studies) |
Conclusion: Presently, there is no strong clinical evidence for causality regarding artificial sweetener use and metabolic health effects, but it is important to examine possible contributions of these common food additives to the global rise in pediatric obesity and diabetes. Main Results: General trend from 6 food intake studies is that artificial sweeteners may reduce total caloric intake when consumed between meals, but when consumed with meals, children may compensate for low-calorie snacks or drinks by increasing meal-associated calories. Data from the 6 epidemiologic studies support the existence of an association between artificially-sweetened beverage consumption and weight gain in children. The few small, randomized controlled trials conducted in children did not find an association between artificial sweetener consumption and weight change. |
|
Miller, 2014 Systematic Review and Meta-Analysis AMSTAR: 8/11 |
All individual LCS (generic and name brands) approved for use globally; food and beverage sources of LCS such as “diet soda”; and sweeteners with different names such as “intense sweetener” or “polyol” At least one measure of body weight or composition |
Up to September 16, 2013 Prospective cohorts and RCTs were eligible if study population was generally healthy (not hospitalized or acutely ill); dose or intake data for at least one LCS (nonnutritive sweetener or polyol) or delivery vehicle of LCS were provided; the effect of LCS, compared with the control arm, could be examined independently of other intervention components; and outcome data for at least one measure of body weight or composition were available |
15 RCTs and 9 prospective cohort studies |
Conclusion: The meta-analysis of observational studies showed a small positive association between LCS intake and BMI, but no association with body weight or fat mass. On the other hand, data from RCTs, which provide the highest quality of evidence for examining the potentially causal effects of LCS intake on body weight, indicate that substituting LCS for calorically dense alternatives results in a modest reduction of body weight, BMI, fat mass and waist circumference. Main Results: In the meta-analysis of all subjects from the RCTs, LCS reduced body weight by 0.80 kg (95% CI: -1.17 to -0.43; fixed-effect weighted group mean differences (WGMD)= -0.61) compared with the comparator arm. In stratified models by age group, LCSs decreased body weight in children (-1.06 kg; 95% CI: -1.57 to -0.30; fixed-effect WGMD= -1.06) and adults (-0.72 kg; 95% CI: -1.15, -0.30; fixed-effect WGMD= -0.52). Analyses by sex showed significant reductions in body weight with LCSs among women (-0.72; 95% CI: -1.19 to -0.25; fixed-effect WGMD= -0.62). The summary estimate for men was null but based on only 2 trials (no evidence of small-study bias was observed). Meta-analyses of the prospective cohort studies were limited largely by differences across the individual studies. Modest statistically significant positive associations between baseline LCS intake and change in BMI (weighted group mean correlations (WGMC): 0.03; 95% CI: 0.01 to 0.06; fixed-effect WGMC=0.03) were observed. In the meta-analysis of LCS intake and weight gain and fat mass no statistically significant associations were observed, and statistical evidence for small-study bias was lacking. |
|
Wiebe, 2011 Systematic Review AMSTAR: 8/11 |
High-intensity caloric sweeteners that are functionally non-caloric Weight change (absolute, BMI) |
1950 – January 2013 Parallel or crossover RCTs comparing sweeteners in generally healthy, overweight/obese and/or diabetic adults (> 16 years) old). Trials had to have at least two groups comparing different sweeteners and at least one week of follow-up. Trials with less than 10 participants were excluded. |
3 RCTs (of the 13 trials looking at weight management, blood glucose and blood lipids, three trials compared a non-caloric sweetener to sucrose; 10 trials compared a saccharide to a different saccharide) |
Conclusion: Although data suggest that non-caloric sweeteners may lead to clinically relevant weight loss through reduced energy consumption; this conclusion was driven by a single trial with a total of 41 participants. Main Results: Two of the three trials reported change in BMI. A four-week trial in healthy participants did not find a significant loss in BMI in non-caloric sweetener recipients (-0.3 kg/m2, 95% CI: -1.1 to 0.5). A 10-week trial in 41 overweight participants found a significantly greater loss in BMI in participants consuming the non-caloric sweetener (-0.9 kg/m2, 95% CI: -1.5 to -0.4). One crossover trial in 10 type 1 diabetic participants found no difference in weight loss between groups over four weeks (0.8 kg, 95% CI: -3.3 to 4.9) |
*A measurement tool for the ‘assessment of multiple systematic reviews’ (AMSTAR)
**Reference overlap: Of the 39 articles included in total across the reviews, 6 were included in two or more reviews.
References Included in Review
- Brown RJ, de Banate MA, Rother KI. Artificial sweeteners: a systematic review of metabolic effects in youth. Int J Pediatr Obes. 2010;5(4):305-12. PMID: 20078374. http://www.ncbi.nlm.nih.gov/pubmed/20078374
- Miller PE, Perez V. Low-calorie sweeteners and body weight and composition: a meta-analysis of randomized controlled trials and prospective cohort studies. Am J Clin Nutr. 2014;100(3):765-77. PMID: 24944060. http://www.ncbi.nlm.nih.gov/pubmed/24944060.
- Wiebe N, Padwal R, Field C, Marks S, Jacobs R, Tonelli M. A systematic review on the effect of sweeteners on glycemic response and clinically relevant outcomes. BMC Med. 2011;9:123. PMID: 22093544. http://www.ncbi.nlm.nih.gov/pubmed/22093544
Supplementary Information:
(Note: One search for low-calorie sweeteners and body weight, type 2 diabetes, cardiovascular disease, and dental caries was conducted. Only reviews on body weight and type 2 diabetes were identified and are presented below.)
Methodology
This question was answered using existing SRs/MA published from January 2010 to August 2014.
Search Strategy for Existing Systematic Reviews/Meta-Analyses
PubMed:
(Non-caloric sweeten* OR non caloric sweeten* OR "Non-Nutritive Sweeteners"[Mesh] OR Non-Nutritive Sweetener*[tiab] OR Non Nutritive Sweetener*[tiab] OR low calorie sweeten* OR (artificial* sweeten*) OR “sugar free” OR sugar-free OR saccharin OR aspartame OR acetosulfame OR sucralose OR trichlorosucrose OR neotame OR erythritol OR rebaudioside* OR rebiana OR diet soda* OR diet drink* OR (intense* sweeten*[tiab]))
pooled analysis* OR systematic[sb] OR systematic review* OR meta-analys* OR meta analys* OR lim to SR/MA
Embase:
(Non-caloric NEXT/1 sweeten*) OR (“non caloric” NEXT/1 sweeten*) OR (Non-Nutritive NEXT/1 Sweeten*) OR “Non-Nutritive” NEXT/1 Sweeten* OR “Non Nutritive” NEXT/1 Sweeten* OR “low calorie” NEXT/1 sweeten* OR (artificial* NEXT/1 sweeten*) OR “sugar free” OR sugar-free OR saccharin OR aspartame OR acetosulfame OR sucralose OR trichlorosucrose OR neotame OR erythritol OR rebaudioside* OR rebiana OR diet soda* OR diet drink* OR (intense* NEXT/1 sweeten*) OR advantame OR (sugar NEXT/1 substitute*) OR stevia OR cyclamate* OR (monk NEXT/1 fruit*)
'systematic review'/exp OR 'meta analysis'/exp OR pooled NEXT/1 analysis* OR “systematic review” OR meta NEXT/1 analys*
Cochrane:
(Non-caloric NEXT/1 sweeten*) OR (“non caloric” NEXT/1 sweeten*) OR (Non-Nutritive NEXT/1 Sweeten*) OR “Non-Nutritive” NEXT/1 Sweeten* OR “Non Nutritive” NEXT/1 Sweeten* OR “low calorie” NEXT/1 sweeten* OR (artificial* NEXT/1 sweeten*) OR “sugar free” OR sugar-free OR saccharin OR aspartame OR acetosulfame OR sucralose OR trichlorosucrose OR neotame OR erythritol OR rebaudioside* OR rebiana OR diet soda* OR diet drink* OR (intense* NEXT/1 sweeten*) OR advantame OR (sugar NEXT/1 substitute*) OR stevia OR cyclamate* OR (monk NEXT/1 fruit*)
Inclusion Criteria
Date Range:
- Published between January 2010 and August 2014 (in English in a peer-reviewed journal)
Study Design:
- Systematic review and/or meta-analysis that included randomized controlled trials and/or prospective cohort studies
Study Subjects:
- Reviews that included studies from high or very high human development (2012 Human Development Index)
- Healthy or at elevated chronic disease risk
Intervention/Exposure:
- Low-calorie sweetener - The Committee approached this topic broadly, including sweeteners labeled as low-calorie sweeteners, non-caloric sweeteners, non-nutritive sweeteners, artificial sweeteners, and diet beverages.
Outcome:
- Body weight: Body mass index, body weight, percent body fat, waist circumference, incidence of overweight or obesity
- Type 2 diabetes: Glucose intolerance, insulin resistance, or incidence of type 2 diabetes
Quality:
- Reviews rated 8-11 on AMSTAR (A measurement tool for the ‘assessment of multiple systematic reviews’)
Search Results
Excluded Articles with Reason for Exclusion
- Althuis MD, Weed DL, Frankenfeld CL. Evidence-based mapping of design heterogeneity prior to meta-analysis: a systematic review and evidence synthesis. Syst Rev. 2014;3:80. PMID: 25055879. http://www.ncbi.nlm.nih.gov/pubmed/25055879. EXCLUDE: Discusses design heterogeneity in SSB research; does not address the question
- Bader JD. Casein phosphopeptide-amorphous calcium phosphate shows promise for preventing caries. Evid Based Dent. 2010;11(1):11-2. PMID: 20348890. http://www.ncbi.nlm.nih.gov/pubmed/20348890. EXCLUDE: Does not examine a low-calorie sweetener (CPP-ACP is a milk-derived product that is intended to remineralize teeth)
- Brahmachari G, Mandal LC, Roy R, Mondal S, Brahmachari AK. Stevioside and related compounds - molecules of pharmaceutical promise: a critical overview. Arch Pharm (Weinheim). 2011;344(1):5-19. PMID: 21213347. http://www.ncbi.nlm.nih.gov/pubmed/21213347. EXCLUDE: Narrative review
- Brown RJ, Rother KI. Non-nutritive sweeteners and their role in the gastrointestinal tract. J Clin Endocrinol Metab. 2012;97(8):2597-605. PMID: 22679063. http://www.ncbi.nlm.nih.gov/pubmed/22679063. EXCLUDE: Narrative review
- Cabrera Escobar MA, Veerman JL, Tollman SM, Bertram MY, Hofman KJ. Evidence that a tax on sugar sweetened beverages reduces the obesity rate: a meta-analysis. BMC Public Health. 2013;13:1072. PMID: 24225016. http://www.ncbi.nlm.nih.gov/pubmed/24225016. EXCLUDE: Examined evidence on SSB tax; does not address the question
- Cohen L, Curhan G, Forman J. Association of sweetened beverage intake with incident hypertension. J Gen Intern Med. 2012;27(9):1127-34. PMID: 22539069. http://www.ncbi.nlm.nih.gov/pubmed/22539069. EXCLUDE: Not a systematic review or meta-analysis (prospective analysis to examine associations between SSBs and ASBs with self-reported incident hypertension)
- Daniels MC, Popkin BM. Impact of water intake on energy intake and weight status: a systematic review. Nutr Rev. 2010;68(9):505-21. PMID: 20796216. http://www.ncbi.nlm.nih.gov/pubmed/20796216. EXCLUDE: Out of scope, systematic review of studies evaluating the impact of drinking water compared with no beverage or other beverages on energy intake and/or weight status
- Franz MJ, Powers MA, Leontos C, Holzmeister LA, Kulkarni K, Monk A, et al. The evidence for medical nutrition therapy for type 1 and type 2 diabetes in adults. J Am Diet Assoc. 2010;110(12):1852-89. PMID: 21111095. http://www.ncbi.nlm.nih.gov/pubmed/21111095. EXCLUDE: Describes medical nutrition therapy for type 1 and type 2 diabetes
- Goyal SK, Samsher, Goyal RK. Stevia (Stevia rebaudiana) a bio-sweetener: a review. Int J Food Sci Nutr. 2010;61(1):1-10. PMID: 19961353. http://www.ncbi.nlm.nih.gov/pubmed/19961353. EXCLUDE: Narrative review
- Keukenmeester RS, Slot DE, Putt MS, Van der Weijden GA. The effect of medicated, sugar-free chewing gum on plaque and clinical parameters of gingival inflammation: a systematic review. Int J Dent Hyg. 2014;12(1):2-16. PMID: 23790138. http://www.ncbi.nlm.nih.gov/pubmed/23790138. EXCLUDE: Examined medicated, sugar-free gum (defined as containing antimicrobial agents or herbal extracts)
- Keukenmeester RS, Slot DE, Putt MS, Van der Weijden GA. The effect of sugar-free chewing gum on plaque and clinical parameters of gingival inflammation: a systematic review. Int J Dent Hyg. 2013;11(1):2-14. PMID: 22747775. http://www.ncbi.nlm.nih.gov/pubmed/22747775. EXCLUDE: dental carries not included as outcome; review focused on comparisons with no chewing gum as a control
- La Vecchia C. Low-calorie sweeteners and the risk of preterm delivery: results from two studies and a meta-analysis. J Fam Plann Reprod Health Care. 2013;39(1):12-3. PMID: 23296849. http://www.ncbi.nlm.nih.gov/pubmed/23296849. EXCLUDE: Did not examine CVD, T2D, body weight, or dental caries as an outcome
- Mallikarjun S, Sieburth RM. Aspartame and risk of cancer: A meta-analytic review. Arch Environ Occup Health. 2013. PMID: 24965331. http://www.ncbi.nlm.nih.gov/pubmed/24965331. EXCLUDE: Did not examine CVD, T2D, body weight, or dental caries as an outcome
- Pereira MA. Diet beverages and the risk of obesity, diabetes, and cardiovascular disease: a review of the evidence. Nutr Rev. 2013;71(7):433-40. PMID: 23815142. http://www.ncbi.nlm.nih.gov/pubmed/23815142. EXCLUDE: Narrative review
- Poolsup N, Pongmesa T, Cheunchom C, Rachawat P, Boonsong R. Meta-analysis of the efficacy and safety of stevioside (from stevia rebaudiana bertoni) in blood pressure control in patients with hypertension. Value in Health. 2012;15(7):A630. EXCLUDE: Examines treatment of blood pressure
- Shankar P, Ahuja S, Sriram K. Non-nutritive sweeteners: review and update. Nutrition. 2013;29(11-12):1293-9. PMID: 23845273. http://www.ncbi.nlm.nih.gov/pubmed/23845273. EXCLUDE: Narrative review
- Ulbricht C, Isaac R, Milkin T, Poole EA, Rusie E, Grimes Serrano JM, et al. An evidence-based systematic review of stevia by the Natural Standard Research Collaboration. Cardiovasc Hematol Agents Med Chem. 2010;8(2):113-27. PMID: 20370653. http://www.ncbi.nlm.nih.gov/pubmed/20370653. EXCLUDE: Focused on treatment